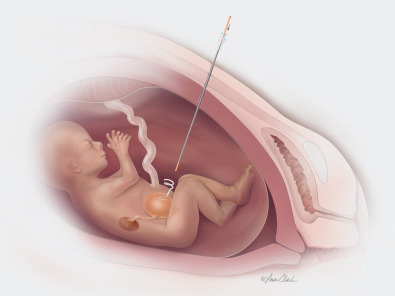
In fetal shunt placement, a shunt (hollow tube) is inserted through the mother’s abdomen and uterus into the fetus to drain fluid from a fluid-filled fetal space into the amniotic cavity.
The most common type of fetal shunt placement is vesicoamniotic shunting for urinary tract blockages, such as bladder outlet obstruction. It also may be used in other conditions that cause buildup of excess fluid that compresses and damages organs, including lungs.
About the procedure
When a fetal urinary tract is blocked completely, the bladder becomes enlarged, and the amount of amniotic fluid decreases (oligohydramnios). This may cause:
• underdeveloped lungs (pulmonary hypoplasia)
• deformities of the face and extremities (Potter sequence)
• kidney damage
A vesicoamniotic shunt creates an alternate pathway for the urine to bypass the obstruction, allowing the urine to drain into the amniotic cavity and restore normal fluid levels.
Before considering fetal shunt placement, an extensive evaluation, including ultrasound, fetal echocardiography serial renal function profile and chromosomal analysis, will be conducted. The procedure is performed in the hospital on an outpatient basis. The mother is given IV sedation, which also sedates the fetus, as well as antibiotics and local anesthesia. Using ultrasound guidance, a metal cannula (tube) on a trochar needle is placed through the mother’s abdomen and uterus, then into the fetal bladder. The trochar is removed, and a drainage catheter is inserted into the cannula, with one end of the catheter in the bladder and the other in the amniotic cavity. The cannula is removed, and correct placement is confirmed by ultrasound.
Amnioinfusion, a surgical procedure that adds fluid to the amniotic sac, may be needed as well.
Risks
Side effects of fetal shunting may include premature labor, trauma to the fetus, separation of the fetal membranes and placental bleeding.